The Ultimate Guide to Decision-Makers and Procurement Power
You’ve developed an innovative surgical robot. Created a breakthrough diagnostic tool. Engineered a lifesaving monitoring system. But none of it matters if you don’t know who buys medical devices for hospitals. This complex web of decision-makers holds the keys to a $500 billion global industry. Whether you’re a manufacturer, distributor, or investor, understanding hospital procurement isn’t just helpful—it’s profit-determining.
I’ve spent 12 years advising medtech companies on hospital sales strategy. The patterns are clear: Those who map the decision hierarchy win contracts. Those who don’t? They bleed cash in endless demos without closing deals. Let’s dissect this ecosystem together.
The Hospital Purchasing Power Grid: Who Really Controls the Budget?
Hospitals operate like micro-governments. Multiple stakeholders wield veto power over purchases. Ignore one faction, and your device dies in committee.
🏢 C-Suite Commanders: The Ultimate Approvers
These executives control the purse strings:
-
Chief Executive Officers (CEOs): Set strategic vision. Prioritize devices aligning with institutional goals (e.g., “Center of Excellence” status).
-
Chief Financial Officers (CFOs): Analyze ROI like forensic accountants. Demand data on:
-
Upfront costs vs. lifetime value
-
Reimbursement impact (DRG adjustments)
-
Staff training expenses
-
-
Chief Medical Officers (CMOs): Clinical evangelists. They ask: “Will this reduce mortality? Improve outcomes? Minimize errors?”
💡 Case Study: A Boston hospital rejected a $2M surgical robot despite surgeon demand. Why? The CFO proved its ROI was 7 years—far exceeding their 3-year threshold.
👩⚕️ Clinical Champions: Department Heads & Key Opinion Leaders
These physicians influence 73% of purchasing decisions (McKinsey):
-
Surgery Chairs: Drive adoption of OR equipment
-
Radiology Directors: Dictate imaging tech purchases
-
ICU Medical Directors: Select monitoring systems
-
Nursing Leadership: Advocate for ergonomic devices reducing staff injury
Pro Tip: Cardiologists often have unusual leverage. Why? Cardiology departments generate ≈20% of hospital revenue (Advisory Board data).
🛡️ Procurement Professionals: The Gatekeepers
These unsung heroes manage the mechanics:
-
Vendor Credentialing: Ensure regulatory compliance
-
Contract Negotiation: Secure bulk pricing through GPOs
-
Supply Chain Optimization: Minimize inventory costs
-
Value Analysis Committees (VACs): 88% of hospitals use these teams to clinically/financially vet devices (AHRMM)
✅ Also check: Pacemaker Cost
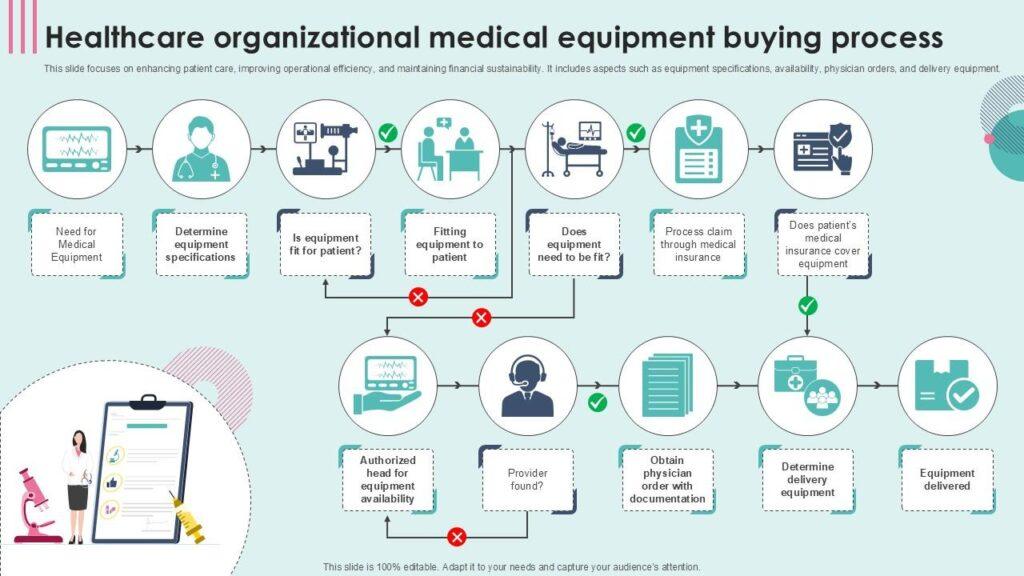
The 7-Stage Hospital Buying Journey: From Need to Implementation
Unlike B2C purchases, hospital procurement follows a ritualized path:
-
Problem Identification
-
Clinicians flag gaps (e.g., “Our infusion pumps have 12% error rates”)
-
Biomedical engineers document equipment failures
-
-
Solution Exploration
-
Committees research options
-
Vendors are invited for demos
-
▶️ Critical: Clinical trials or peer-reviewed data requested
-
-
Budget Blessing
-
CFOs evaluate:
-
Capital expenditure vs. operating lease options
-
Group Purchasing Organization (GPO) contract availability
-
-
⚠️ 67% of projects die here due to funding gaps (Sg2)
-
-
Vendor Thunderdome
-
Head-to-head trials (e.g., Device A vs. Device B on 50 patients)
-
Scoring rubrics weighting:
-
Clinical efficacy (30%)
-
Total cost of ownership (25%)
-
Service support (20%)
-
Training simplicity (15%)
-
EHR integration (10%)
-
-
-
Contract Siege Warfare
-
6-18 month negotiations covering:
-
Bulk pricing tiers
-
Service Level Agreements (SLAs)
-
Penalty clauses for downtime
-
-
-
Implementation Marathon
-
Staged rollouts (e.g., pilot units → full deployment)
-
Biomedical engineering sign-off
-
-
Post-Purchase Vigilance
-
Usage monitoring (“Are doctors actually using it?”)
-
Outcome tracking (Readmission reductions? Complication rates?)
-
✅ Also check: Medical Device ROI
Selling Secrets: How Top Medtech Reps Win Hospital Contracts
Relationship Architecture
-
Physician Access:
-
Sponsor CME courses on relevant clinical topics
-
Fund residency programs (creates future advocates)
-
-
Administrator Alignment:
-
Host “Economic Summit” dinners showing cost-per-case savings
-
Offer facility assessments (e.g., “OR Efficiency Review”)
-
Proposal Alchemy
Transform generic pitches into irresistible offers:
| Weak Section | Power Upgrade |
|---|---|
| “Our scanner has high resolution” | “Reduces repeat scans by 40%—saving $217K annually at your volume” |
| “Easy to use” | “Cuts radiologist burnout by 15 hours/month (validated at Mass General)” |
| “Competitive pricing” | “Total 5-year cost: $1.2M vs. $1.9M for Device X—see audited TCO model” |
GPO Navigation Mastery
Group Purchasing Organizations influence 80% of hospital spending. Tactics:
-
IDN Leverage: Partner with Integrated Delivery Networks to pressure GPOs
-
Tiered Commitments: Offer discounts for market share thresholds
-
Consignment Models: Eliminate upfront costs (hospitals pay per use)
✅ Also check: Pay-Per-Treatment Pricing
5 Costly Myths About Hospital Procurement (Debunked)
-
“Price is the #1 Factor”
Reality: Clinical outcomes dominate. A $500K device reducing surgical complications pays for itself in 90 days. -
“Physicians Make Solo Decisions”
Reality: 92% of purchases require cross-functional consensus (ECRI Institute). -
“GPO Contracts Guarantee Sales”
Reality: GPOs enable purchasing—they don’t mandate it. Local VACs still veto 40% of GPO-listed items. -
“Newer Tech Always Wins”
Reality: Legacy systems have inertia. One hospital used 30-year-old monitors because “nurses know the beeps.” -
“Hospitals Pay List Price”
Reality: Academic medical centers extract 50-70% discounts through capitated deals.
✅ Also check: Morpheus8 Price Comparisons
Future Shock: 2025+ Procurement Shifts
🤖 AI-Powered Purchasing
-
Predictive algorithms forecasting device failures
-
Real-time usage analytics triggering auto-reorders
-
Example: Cleveland Clinic’s AI reduces inventory waste by 31%
♻️ Sustainability Mandates
-
Carbon footprint disclosures required for RFPs
-
Preference for reusable devices (e.g., reprocessed scopes)
-
Stat: 68% of providers now include ESG criteria in purchasing (Deloitte)
🧩 Modular Equipment
Hospitals favor scalable systems like:
-
Ultrasound carts adding AI diagnostic modules
-
OR “towers” with swappable components
-
✅ Also check: Ultrasound Machine Innovations
Real-World Wins: How Companies Broke Into Top Hospitals
Case 1: The $23M Imaging Deal
Challenge: A startup’s MRI needed to displace an incumbent at Mayo Clinic.
Strategy:
-
Funded a 200-patient study showing 22% faster scan times
-
Structured lease-to-own financing via Siemens Financial
-
Trained 94% of radiology techs pre-installation
Result: 5-year system-wide contract.
Case 2: Infection-Control Catheter
Challenge: Get ICU adoption despite 40% cost premium.
Tactics:
-
Mapped cost of central-line infections ($48K/case)
-
Partnered with hospital epidemiologists on trial design
-
Offered 90-day money-back guarantee
Outcome: 300+ hospital deployments in 18 months.
✅ Also check: Viora V20 Before/After Results
FAQs: Hospital Procurement Unfiltered
Q: How long do decisions REALLY take?
A: Capital equipment: 9-24 months. Disposables: 3-6 months. Teaching hospitals move slowest.
Q: Do bribes or kickbacks happen?
A: Stark/Anti-Kickback laws make this radioactive. But “consulting fees” to physicians still draw scrutiny.
Q: Can startups compete without GPO contracts?
A: Yes—pilot programs with progressive IDNs. Target “innovation committees” at academic centers.
Q: What’s the #1 reason good devices fail?
A: Poor EHR integration. Nurses will boycott tech that adds charting time.
Q: How do I find key contacts?
A: LinkedIn > Title searches: “Value Analysis Coordinator,” “Director, Supply Chain”.
The medical device gold rush isn’t ending—it’s accelerating. By 2027, the market hits $800B (Grand View Research). But the winners won’t just have superior tech. They’ll master the art of navigating who buys medical devices for hospitals.
Ready to equip your success? Explore our marketplace of hospital-grade devices vetted by clinical and procurement experts:
👉 Discover Revenue-Driving Medical Technology
✅ Also check: FDA-Approved Portable Oxygen Concentrators
✅ Also check: Best Fall Detection Devices